I'M HOME FROM THE EMERGENCY ROOM!
- StHooch
- Mar 14, 2022
- 4 min read
It's been a long week. I'm home now and will post everything I know about what is going on with me and Demetrius.

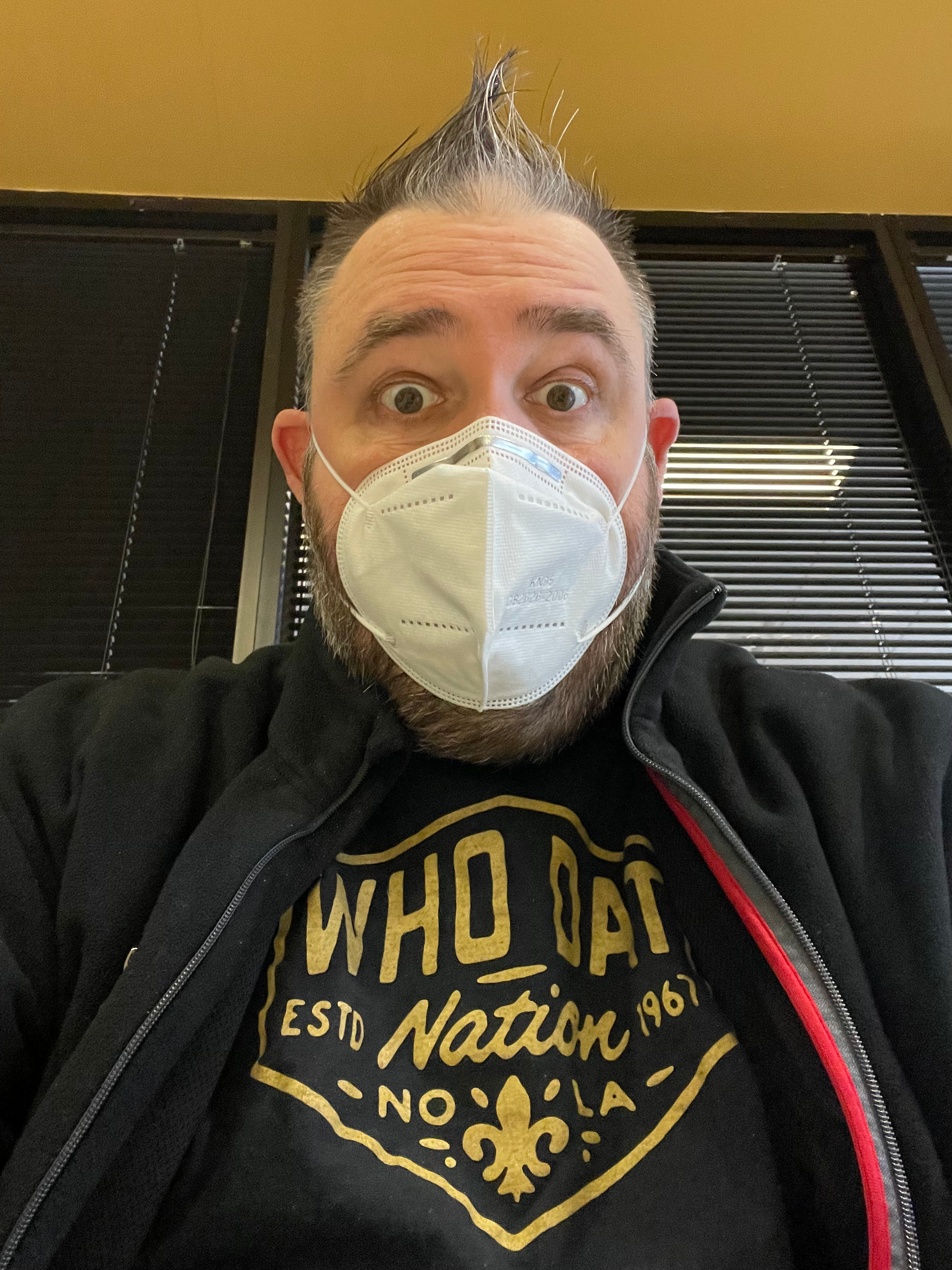
So, what is it? Let's start from last Thursday. I woke up that morning in a lot of abdominal pain. Ashley and I were given the advice by transplant to call 9-1-1 and head in to the emergency room. We were in the ER for hours (called ambulance in the late morning and arrived in room right after 11:00pm) before a room was ready for me to be admitted. Once admitted, I was hooked up to fluids and found out that I was extremely dehydrated. I only had a few small things to eat and only water with my meds over three days leading up to this episode. Staying hydrated is extremely important for transplant patients and I new it but I felt sick to my stomach with zero appetite.
Earlier in the week I saw a specialist and they thought it was a bacterial infection. I gave this information to the nurses in addition to informing them I was recently diagnosed with gastroparesis. Collecting labs, giving me fluids and giving me meds for nausea continued for the first 48-hours. We asked for updates in a non-annoying way and were given zero information. I figured it was a really bad case of gastroparesis and it seemed that way for a bit. TO make sure there was nothing wrong inside of me they decided to go ahead and do the scope to look inside my stomach to look for blockage or any other concerns. It was time for...THE SCOPE!
THE SCOPE. Gastroscopy is a medical term that has two parts: gastro for "stomach," and scopy for "looking." Gastroscopy, then, is a diagnostic test that enables the doctor to look inside your stomach. The instrument used to perform this simple test is the gastroscope; a long, thin, flexible fiberoptic tube.
After the test, they quickly ruled out a bacterial infection to to my white blood cell count only being slightly elevated. Once the nausea stopped, they then focused on my weakness and dizziness when I stood up or tried to walk. This was very concerning, as it should be considering not too many people can catch a 6'5" 267lb. man. It was quickly discovered I was experiencing "Orthostatic hypotension."
"Orthostatic hypotension — also called postural hypotension — is a form of low blood pressure that happens when you stand up from sitting or lying down. Orthostatic hypotension can make you feel dizzy or lightheaded, and maybe even cause you to faint."
Saturday, March 12th
Being in bed for three days, I was getting cabin fever. The stomach cramping and nausea were under control with medications. The bloating and low blood pressure were still an issue but manageable at home. I was glad to hear this. I was ready to go home. Just need clearance from the various departments to get my discharge. We waited in the room to see the last doctor. We waited. He arrived. We got the news.
The News
The doctor explained that they really had no conclusive evidence of what exactly was going on. He could only say that he felt that it could be a really bad case of gastrparesis and that I could manage it with diet and possibly meds. Since he did not know 100% what was going on, he recommended that I get a HIDA scan.
A hepatobiliary iminodiacetic acid (HIDA) scan is an imaging procedure used to diagnose problems of the liver, gallbladder and bile ducts. For a HIDA scan, also known as cholescintigraphy or hepatobiliary scintigraphy, a radioactive tracer is injected into a vein in your arm.
He then gave me two suggested options:
Option One: Stay in the hospital for two more nights to wait to have the scan Monday morning and get results to see if I needed to stay longer.
Option Two: Get discharged and call to schedule an appointment to get the scan on Monday. This would require pre-authorization from insurance making this option more time consuming.
Ashley and I talked about it and decided that I needed to stay to expedite the scan. I then hung out in the hospital to ONLY wait for the scan on Monday. Thank goodness I had my phone.
Monday, March 14th
The scan took two hours to complete. They injected me with radiation and I had to stand in front of the scanner every ten minutes to see how the radiation was progressing through my digestive system. After the second time standing up I had tunnel vision and felt like I was about to pass out so we did the remainder of the scan laying down. After the first hour, I had to drink a chocolate flavored Nestle Boost shake to activate my gall bladder. After drinking the shake I had to have pics taken every 20 minutes. After we were done it was back to the room.
At this point it was 11:00am and we were told that the results may not be reviewed up until 6:00pm. >sigh< The Gastro Doc finally came back around 2:00pm with the results.
The Results
Everything from the scan looked fantastic...except for one thing. My gallbladder was not emptying as fast as it should and is only operating at 19%.
I will be contacted this week to schedule a consultation to have an outpatient procedure to remove my gallbladder. It is possible that this will alleviate some o my symptoms or they could vanish completely. Of course this is in addition to changing my diet.
None of this affects or is directly related to the kidney transplant.
It really amazes me that it was a last minute test at the end that discovered this finding the real problem. I am doing much better at home with my new diet of eating six to eight small snacks/meals per day with lots of fluids between meals.
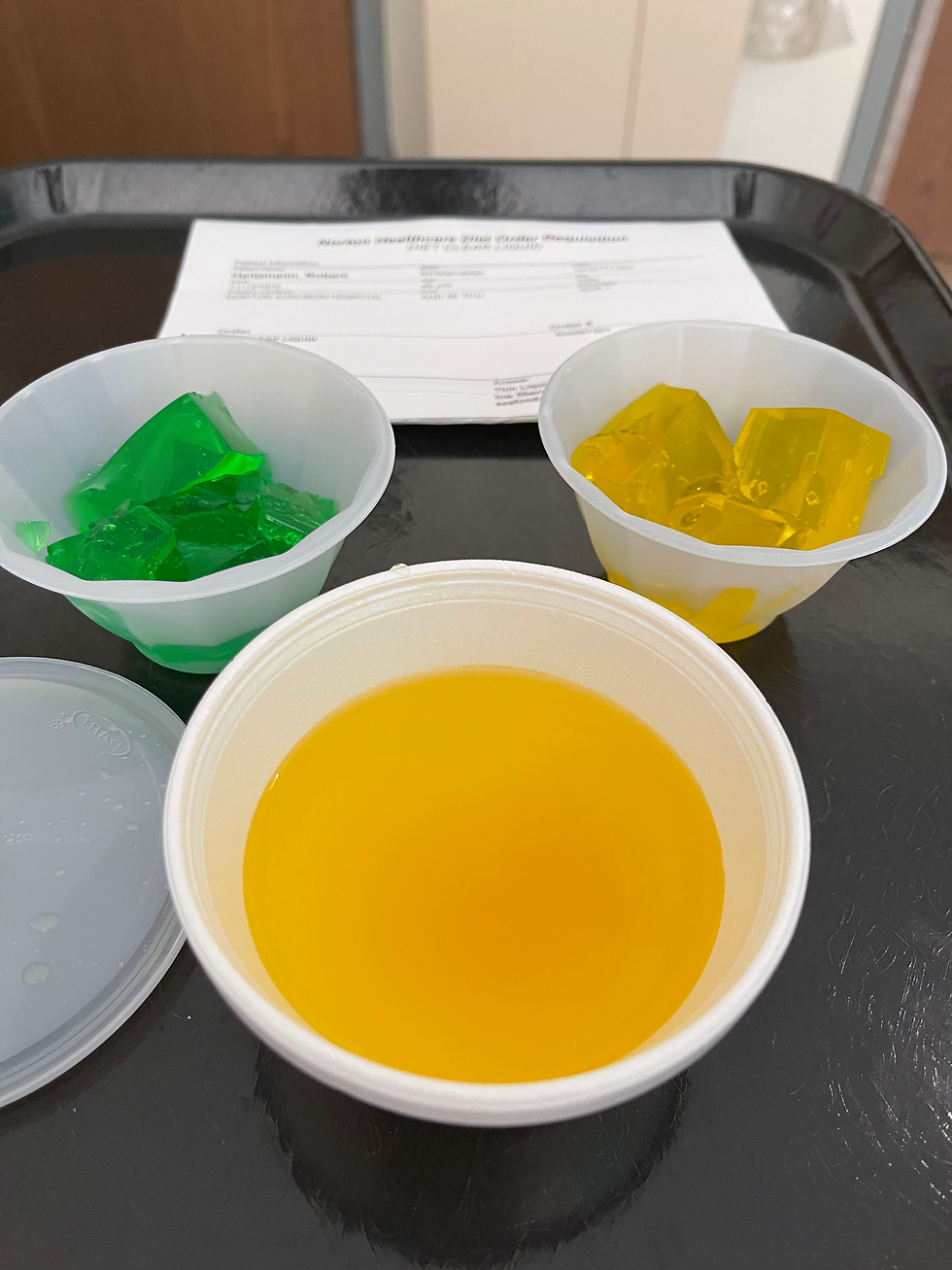
As always, I really appreciate the support I have gained from friends, family and complete strangers. This has been a ride and hopefully soon we will finally get to the fun part! In closing, I have included of the best and worst meals I had while at Norton Audubon Hospital. Enjoy!


Comments